 Secretory IgA (sIgA) is a biomarker that may reflect the impact of stress on the immune system as well as the resilience of the immune response. Secretory IgA is synthesized by activated B cells along mucosal membranes in the oral cavity, nasal passages, ocular surfaces, gastrointestinal tract, respiratory tract, and the genitourinary tract. Since these mucosal surfaces are exposed to the outside world, sIgA is considered to be an important part of the first line of immune defense against the pathogens that cause infections.
Secretory IgA (sIgA) is a biomarker that may reflect the impact of stress on the immune system as well as the resilience of the immune response. Secretory IgA is synthesized by activated B cells along mucosal membranes in the oral cavity, nasal passages, ocular surfaces, gastrointestinal tract, respiratory tract, and the genitourinary tract. Since these mucosal surfaces are exposed to the outside world, sIgA is considered to be an important part of the first line of immune defense against the pathogens that cause infections.
When present in mucosal secretions, sIgA molecules bind to infectious pathogens, thus preventing their adhesion and entrance into the body. The binding of sIgA molecules to these pathogens then facilitates their elimination. Preventing the adhesion and adsorption of pathogenic organisms, while also facilitating their removal, is a phenomenon known as “immune exclusion.” Two additional methods by which sIgA molecules reduce the likelihood of infection include direct interference with surface receptor binding and reduction in the activation or expression of pathogenic virulence factors.
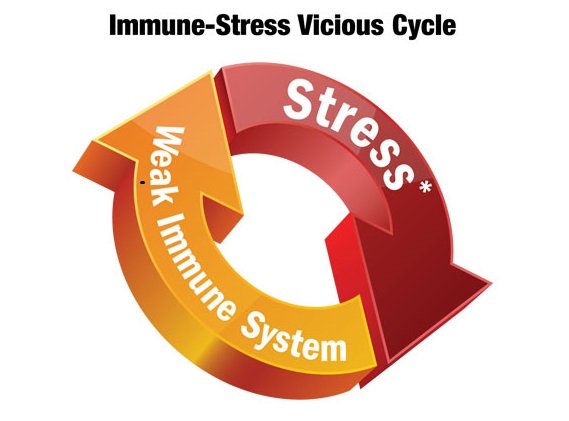
Secretory IgA production can be suppressed by stress and elevated cortisol levels. When the cortisol level is chronically elevated, sIgA production decreases, leading to an inadequate immune response which then, ultimately, increases the risk of infection. The total salivary sIgA level generally mirrors the sIgA level in other mucosal tissues (e.g., lungs) and is an expedient tool to monitor changes in mucosal immune status.
Two new resources have been posted on the Provider Tools page to assist with the clinical interpretation of sIgA levels and treatment considerations to optimize sIgA production.
The following resources are now available:
- Secretory IgA Interpretive Guide
- Treatment Considerations to Support Optimal sIgA Production
DiagnosTechs providers may log in to access these new resources on our Provider Tools webpage!