
Introducing the Cortisol Awakening Response Test: A Tool for Managing Chronic Stress, Depression, Obesity, and Type 2 Diabetes

As discussed in a previous article, cortisol is known as the stress hormone because stress significantly affects the amount of cortisol released by the adrenal glands. While acute stress tends to significantly increase cortisol production, cortisol is also produced during non-stressful times and is crucial for the optimal function of the body every day. In healthy individuals, cortisol levels naturally shift throughout the day in a pattern known as a diurnal rhythm. A diurnal rhythm is a circadian rhythm that is repeated every 24 hours and synchronized with the day/night cycle.1
Here is an example of a healthy diurnal rhythm:
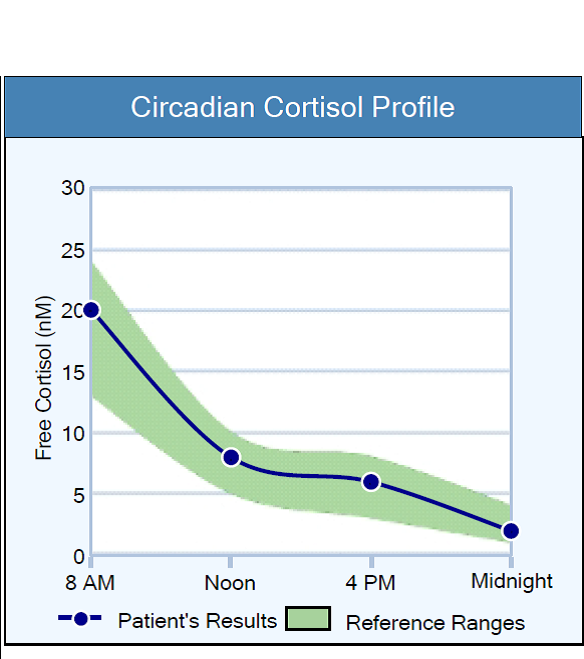
A unique and dramatic component of the 24-hour cortisol diurnal rhythm is the Cortisol Awakening Response (CAR). The CAR was first described in the 1990s and provides insight into the health of the hypothalamic-pituitary-adrenal (HPA) axis. During a normal day, the most substantial shift in the cortisol level occurs during the CAR.2
In a healthy individual, the daily cortisol level peaks 30–45 min post-awakening, and the cortisol level should increase by at least 50% during the CAR compared to the cortisol level at awakening.3 The CAR is significantly larger following morning awakenings compared to afternoon awakenings. Research shows the CAR tends to be absent after an evening nap, suggesting the overall circadian rhythm of the HPA axis and the influence of light during morning awakenings both play a role in the amplitude of the CAR.4
An abnormal CAR can be either heightened or blunted, and the magnitude of the CAR correlates with neuropsychiatric and metabolic health conditions.2 According to research, an abnormal CAR is associated with several health concerns, including obesity, clinical depression, chronic stress, and type 2 diabetes.5
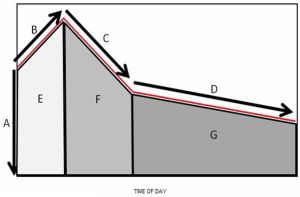
Image credit: Champaneri S, Xu X, Carnethon MR, et al. Diurnal salivary cortisol and urinary catecholamines are associated with diabetes mellitus: the Multi-Ethnic Study of Atherosclerosis. Metabolism. 2012;61(7):986-995. doi:10.1016/j.metabol.2011.11.006
“A”, “B”, and “C” in the image above demonstrate the powerful Cortisol Awakening Response (CAR), which is a dramatic and natural part of the daily diurnal cortisol rhythm.
“A” in the image above is the salivary cortisol level at time zero, which is the time of awakening. “B” is the significant rise in the salivary cortisol level during the CAR, which occurs approximately 30-45 minutes after awakening. “C” is the natural decrease in the salivary cortisol level after the CAR. “D” depicts the decline in the salivary cortisol level that occurs between morning and bedtime.6

The Cortisol Awakening Response Test and Obesity
While the data conflicts at times, adults with obesity often display a blunted diurnal pattern, which manifests as decreased cortisol variability, lower morning cortisol levels upon awakening, higher cortisol levels in the evening, and a smaller overall change in cortisol levels throughout the day.7
Champaneri et al. determined there is a direct association between the diurnal cortisol profile and abdominal obesity that is independent of demographics, socioeconomic status, medications, and smoking. The study included over 6,800 men and women who were 45 to 84 years of age. According to the analysis, there was a significant negative association between the cortisol awakening response and both body mass index (BMI) and waist circumference (WC). A negative or inverse association means the higher the BMI and the larger the waist circumference, the more blunted the cortisol awakening response. These findings are consistent with several other studies that also included a large number of participants.8
A clinical trial by Yu et al. demonstrated obese children also have a dampened or blunted circadian cortisol rhythm characterized by a flat cortisol awakening response and less sharply declining cortisol levels between awakening and bedtime. The severity of the blunting directly correlated with heavier weight in the study participants. Dysfunction in the HPA axis is a known risk factor for metabolic diseases, such as obesity, and is closely related to negative health outcomes. Therefore, testing and stabilizing circadian cortisol rhythms could be an effective approach to preventing childhood obesity, according to the authors of the study.7
The Cortisol Awakening Response Test and Type 2 Diabetes
There is a significant association between blood sugar management and cortisol. In addition to many other beneficial effects throughout the body, cortisol increases blood sugar levels as needed for energy production throughout the day. When cortisol levels are chronically elevated, though, they can increase blood glucose levels too much, induce insulin resistance, and contribute to the development of type 2 diabetes. When tested, those with diabetes tend to have higher baseline cortisol levels and higher cortisol output over 24 hours. Thus, the data suggests dysregulation of the HPA axis is associated with diabetes.6,9
The results of research on the CAR in those with diabetes have been mixed, though the association is becoming clearer and more refined as larger research studies are published.6,9,10 According to the latest data, the CAR is blunted in those with diabetes compared to those without diabetes; however, this association appears to be more significant in men and Caucasian populations.6,9-13
Research suggests unhealthy changes in the cortisol circadian rhythm could occur before the development of diabetes. Therefore, maintaining a healthier and more robust CAR could prevent the progression toward abnormal blood sugar metabolism and diabetes.12 A blunted CAR and flattening of the diurnal cortisol curve, which indicates hypothalamic–pituitary–adrenal (HPA) axis dysregulation, is also associated with insulin resistance, depression, and stress.14
The Cortisol Awakening Response Test and Clinical Depression
Like type 2 diabetes, studies examining the association between the CAR and clinical depression have found that an abnormal CAR is significantly associated with depression, but the specifics of the association are still unclear. Some studies report a blunted CAR in depressed patients, whereas others report an increased or exaggerated CAR. Recent research, however, suggests that the CAR could be dependent upon the severity of the depression. Mild to moderate depression appears to be associated with a normal or heightened CAR, while severe or chronic depression is associated with a blunted CAR.15
Researchers suggest that a long period of mental or physical stress, such as clinical depression, may reduce the number or sensitivity of cortisol receptors so that the HPA axis becomes less responsive.15,16 Elevated cortisol levels for a prolonged period due to the decreased sensitivity might eventually contribute to lower cortisol levels, which could explain the shift in the CAR as the severity of depression increases.15
There is speculation the CAR could be a sensitive test to capture biological vulnerability to depression, and some clinicians refer to the CAR as “an index of one’s overall vulnerability to depression.”3 Researchers also suggest a “flexible CAR,” characterized by a lower CAR on weekends and higher CAR on weekdays, as expected in a healthy population, could be associated with successful coping and a resilient psychological profile.15
The Cortisol Awakening Response Test and Chronic Stress
Chronic stress is defined as repeated or constant exposure to psychological stressors. Chronic stress can significantly impact mental and physical health, as we have discussed in previous articles. One of the biological processes thought to contribute to the association between chronic stress and well-being is the dysfunction of the hypothalamic-pituitary-adrenal (HPA) axis.17
Given the increased interest in mind-body medicine and understanding the significant links between chronic stress and health, many researchers are assessing the clinical usefulness of tests that can provide quantitative measures of stress-related alterations in biological processes.17
Cortisol has been identified and recommended as an HPA axis marker by the National Institute of Nursing Research (NINR).17 The HPA axis is the most important neuroendocrine stress system, and the cortisol awakening response (CAR) is a core biomarker of HPA axis regulation.18 A flattened or blunted CAR is one of the most reliable and consistent markers of HPA axis dysfunction.19
Duan et al. investigated the effect of chronic stress on the CAR in healthy young men studying for a major examination in China. An academic exam is a substantial stress for students in China that results in high psychological and physiological strain. To pass the examination, the young participants in the study spent an average of 9.6 hours studying each day for approximately six months.20
The results demonstrated that self-reported perceived stress and anxiety levels were significantly higher in the examination group. Moreover, the CAR of the examination group was blunted compared to the non-exam control group, and this blunting effect was most pronounced in the participants who reported the highest levels of perceived stress.20
Several other studies have confirmed an association between a blunted CAR and stress-related disorders, such as burnout, PTSD, cognitive deficits, and chronic fatigue syndrome.20,21 Research data also show a decreased CAR is present in chronically stressed caregivers and middle-aged women who have high chronic economic hardship or job-related stress.20
The Cortisol Awakening Response Test, Stress Management, and Preventing Chronic Disease
The results of the Cortisol Awakening Response Test could support the prescription of a customized and clinically effective stress management protocol to significantly improve the health of the HPA axis and adrenal glands. An optimal Cortisol Awakening Response and healthy cortisol levels may also reduce the risk of developing obesity, type 2 diabetes, depression, and many other chronic health concerns, according to the latest research.
Consider testing salivary cortisol levels in your patients today. To special order a Cortisol Awakening Response Test, you may use an Adrenal Stress Index test kit and add 2 extra vials for saliva collection at 30 minutes and 60 minutes post-awakening. These 2 extra vials are collected after the regular MORNING saliva vial. You may indicate this special order on the Adrenal Stress Index order form by adding 2 extra cortisol tests with the times “30 minutes” and “60 minutes” specified on the form.
To place a test order, click here. As a reminder, DiagnosTechs can drop ship test kits directly to your patients. You may select this option at the top of the order form.
Please visit our Provider Tools page for information about adrenal restoration, testing guidelines, and more.
YOU MAY ALSO ENJOY
Most of us think of melatonin as the hormone that is required for optimal sleep. While this is true, melatonin also has a variety of other beneficial effects beyond sleep. Melatonin is known to affect the immune system, bone health, fertility, mitochondrial function, and more. Since melatonin does have a profound impact on many different organs and tissues, it is important to test your natural melatonin levels and be mindful of them when thinking about supplementing with this fascinating hormone.
April is Stress Awareness Month, so let’s learn more about the stress hormone known as cortisol! While cortisol is known as the stress hormone, it is crucial for the optimal function of your body every day. In healthy individuals, cortisol levels naturally shift throughout the day in a pattern known as a diurnal rhythm.
THE BENEFITS OF SALIVA HORMONE TESTING
If you could choose, would you rather spit into a tube or have a needle jabbed into your arm to measure your hormone levels? We suspect you would rather not get stuck with a needle, and you do have a choice! Saliva hormone testing offers many benefits, including painless collection in the comfort of your home at any time. Saliva hormone tests can help determine the underlying cause(s) of PMS, insomnia, anxiety, fatigue, infertility, migraines, weight gain, hot flashes, hair loss, and many other health concerns.
SYNERGISTIC NUTRIENTS FOR ADRENAL SUPPORT
Chronic stress is a frequent underlying cause of low nutrient levels and health issues. In fact, according to the World Health Organization (WHO), approximately 450 million people worldwide are affected by stress-related disorders. Research indicates stress could be responsible for an estimated 70% of visits to primary care providers, which is shocking. Fortunately, the consistent use of a synergistic blend of vitamins, minerals, and herbal extracts that nourish the adrenal glands could support a healthy stress response.
References:
- Hedge A. Biological Rhythms – Cornell University. Cornell University Ergonomics Web. Published August 2013. Accessed March 31, 2023.
- Stalder T, Kirschbaum C, Kudielka BM, et al. Assessment of the cortisol awakening response: Expert consensus guidelines. Psychoneuroendocrinology. 2016;63:414-432. doi:10.1016/j.psyneuen.2015.10.010
- Adams GC, Wrath AJ, von Dewitz B, et al. Attachment impacts cortisol awakening response in chronically depressed individuals. Psychoneuroendocrinology. 2020;120:104778. doi:10.1016/j.psyneuen.2020.104778
- Elder GJ, Wetherell MA, Barclay NL, Ellis JG. The cortisol awakening response–applications and implications for sleep medicine. Sleep Med Rev. 2014;18(3):215-224. doi:10.1016/j.smrv.2013.05.001
- Golden SH, Sánchez BN, Wu M, et al. Relationship between the cortisol awakening response and other features of the diurnal cortisol rhythm: the Multi-Ethnic Study of Atherosclerosis. Psychoneuroendocrinology. 2013;38(11):2720-2728. doi:10.1016/j.psyneuen.2013.06.032
- Champaneri S, Xu X, Carnethon MR, et al. Diurnal salivary cortisol and urinary catecholamines are associated with diabetes mellitus: the Multi-Ethnic Study of Atherosclerosis. Metabolism. 2012;61(7):986-995. doi:10.1016/j.metabol.2011.11.006
- Yu T, Zhou W, Wu S, et al. Evidence for disruption of diurnal salivary cortisol rhythm in childhood obesity: relationships with anthropometry, puberty and physical activity. BMC Pediatr. 2020;20(1):381. doi:10.1186/s12887-020-02274-8
- Champaneri S, Xu X, Carnethon MR, et al. Diurnal salivary cortisol is associated with body mass index and waist circumference: the Multiethnic Study of Atherosclerosis. Obesity (Silver Spring). 2013;21(1):E56-E63. doi:10.1002/oby.20047
- Dias JP, Joseph JJ, Kluwe B, et al. The longitudinal association of changes in diurnal cortisol features with fasting glucose: MESA. Psychoneuroendocrinology. 2020;119:104698. doi:10.1016/j.psyneuen.2020.104698
- Chan K, Wong FS, Pearson JA. Circadian rhythms and pancreas physiology: A review. Front Endocrinol (Lausanne). 2022;13:920261. doi:10.3389/fendo.2022.920261
- Lederbogen F, Hummel J, Fademrecht C, et al. Flattened circadian cortisol rhythm in type 2 diabetes. Exp Clin Endocrinol Diabetes. 2011;119(9):573-575. doi:10.1055/s-0031-1275288
- Kluwe B, Ortiz R, Odei JB, et al. The association of cortisol curve features with incident diabetes among whites and African Americans: The CARDIA study. Psychoneuroendocrinology. 2021;123:105041. doi:10.1016/j.psyneuen.2020.105041
- Bruehl H, Wolf OT, Convit A. A blunted cortisol awakening response and hippocampal atrophy in type 2 diabetes mellitus. Psychoneuroendocrinology. 2009;34(6):815-821. doi:10.1016/j.psyneuen.2008.12.010
- Joseph JJ, Golden SH. Cortisol dysregulation: the bidirectional link between stress, depression, and type 2 diabetes mellitus. Ann N Y Acad Sci. 2017;1391(1):20-34. doi:10.1111/nyas.13217
- Neyer S, Witthöft M, Cropley M, et al. The cortisol awakening response at admission to hospital predicts depression severity after discharge in major depressive disorder patients-A replication study. Front Neurosci. 2022;16:952903. doi:10.3389/fnins.2022.952903
- Gaffey AE, Walsh EC, Ladd CO, et al. Alterations in Systemic and Cognitive Glucocorticoid Sensitivity in Depression [published correction appears in Biol Psychiatry Cogn Neurosci Neuroimaging. 2019 Mar;4(3):326]. Biol Psychiatry Cogn Neurosci Neuroimaging. 2019;4(3):310-320. doi:10.1016/j.bpsc.2018.11.007
- Salomon RE, Tan KR, Vaughan A, et al. Minimally-invasive methods for examining biological changes in response to chronic stress: A scoping review. Int J Nurs Stud. 2020;103:103419. doi:10.1016/j.ijnurstu.2019.103419
- Boehringer A, Tost H, Haddad L, et al. Neural Correlates of the Cortisol Awakening Response in Humans. Neuropsychopharmacology. 2015;40(9):2278-2285. doi:10.1038/npp.2015.77
- Basson R, O’Loughlin JI, Weinberg J, et al. Dehydroepiandrosterone and cortisol as markers of HPA axis dysregulation in women with low sexual desire. Psychoneuroendocrinology. 2019;104:259-268. doi:10.1016/j.psyneuen.2019.03.001
- Duan H, Yuan Y, Zhang L, et al. Chronic stress exposure decreases the cortisol awakening response in healthy young men. Stress. 2013;16(6):630-637. doi:10.3109/10253890.2013.840579
- Law R, Clow A. Stress, the cortisol awakening response and cognitive function. Int Rev Neurobiol. 2020;150:187-217. doi:10.1016/bs.irn.2020.01.001





